New treatment of irritable bowel syndrome by autonomic nervous system remodeling :
Irritable Bowel Syndrome (IBS), is classified as a functional gastrointestinal disease. Autonomic nervous system remodeling by limbic rehabilitation is a very sophisticated technique allowing a physiological treatment of bowel diseases . In cases of “pure irritable bowel syndrome” the efficiency of the treatment is now confirmed (hundreds of patients successfully treated) it’s also the same in IBS associated with nonspecific colitis. Now we begin to try successfully the IBD patients. To understand the efficacy of this technic we must begin to study the etiology and the exact mechanism leading to these abnormalities. IBS, is a chronic condition of the lower gastrointestinal tract that affects as many as 15% of adults in the world. Not easily characterized by structural abnormalities, infection, or metabolic disturbances, the underlying mechanisms of IBS remained for many years unclear.Recent research, however, has lead to an increased understanding of IBS. As a result, IBS is often referred to as spastic, nervous or irritable colon. Its hallmark is abdominal pain or discomfort associated with a change in the consistency and/or frequency of bowel movements.
The frequency of IBS in any given population depends, in part, on the ethnic and cultural background of the population being studied, and the criteria used to diagnose the disease. Eight to 20% of adults in the Western world report symptoms consistent with IBS (approximately 65% of these are women). Asia and Africa have similar rates to those in the Western world in general. In India IBS is more common among men, although it is possible that this is a result of differences in symptom reporting and health care use between genders.
The symptoms of IBS may include abdominal pain, distention, bloating, indigestion and various symptoms of defecation. There are three subcategories of IBS, according to the principal symptoms. These are pain associated with diarrhea; pain associated with constipation; and pain and diarrhea alternating with constipation. IBS is not a psychiatric disorder, although it is tied to emotional and social stress, which can affect both the onset and severity of symptoms. IBS patients suffer from a disproportionately higher rate of co-morbidity with other disorders, such as fibromyalgia, chronic fatigue, pelvic pain and psychiatric disorders. The primary features of the syndrome include motility, sensation and central nervous system dysfunction. Motility dysfunction may be manifest in muscle spasms; contractions can be very slow or fast. An increased sensitivity to stimuli causes pain and abdominal discomfort. Researchers also suspect that the regulatory conduit between the central and enteric pathway in patients suffering from IBS may be impaired. Research suggests that many patients with Irritable Bowel Syndrome have disorganized and appreciably more intense colonic contractions than normal controls.
Pathophysiology :
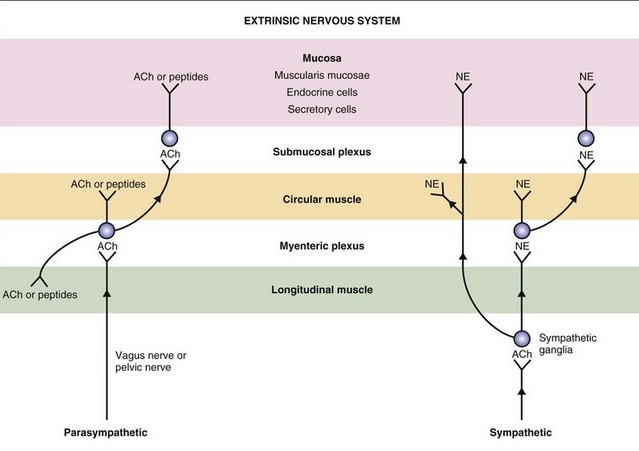
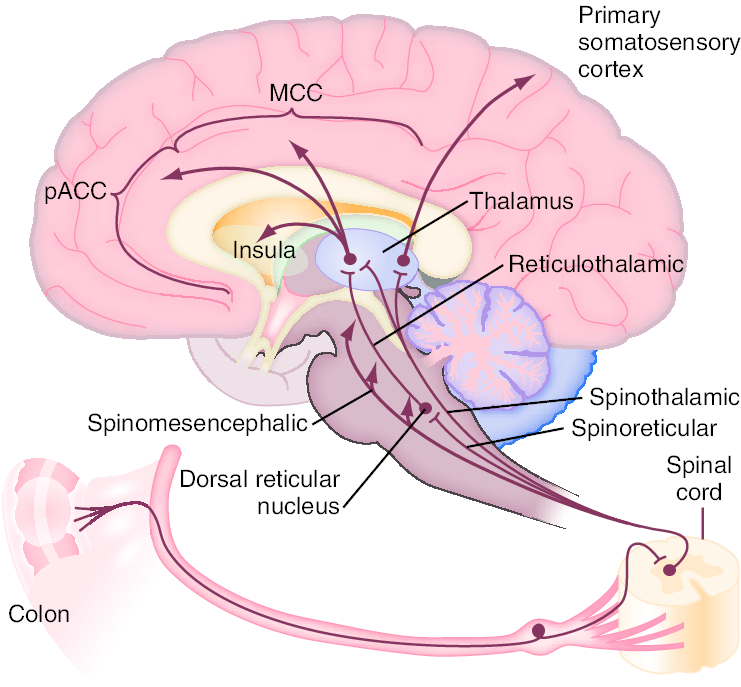
Enteric propulsion and sensation are, in part, mediated by acetylcholine and serotonin (5HT). The physiology of sensation in the gut is multifaceted. Entero-endocrine cells transmit mechanical and chemical messages. The communication between gut and brain results in reflex responses mediated at three levels—prevertebral ganglia, spinal cord and brainstem. 5-HT, substance P, CGRP, norepinephrine, kappa opiate and nitric oxide are all involved in the perception and autonomic response to visceral stimulation. Sensation is conveyed from the viscus to the conscious perception via neurons in vagal and parasympathetic fibers. Afferent nerves in the dorsal root ganglion synapse with neurons in the dorsal horn. These signals result in reflexes that control motor and secretory functions as they synapse with efferent paths in the prevertebral ganglia and spinal cord. Pain is processed through spinal afferents in the dorsal horn. Ultimately, stimulation of the brainstem brings sensation to a conscious level :
Bidirectional signaling between the brainstem and the dorsal horn mediate sensation. The descending pathways are primarily adrenergic and serotonergic and affect incoming stimuli. End organ sensitivity, stimulus intensity changes or receptive field size of the dorsal horn neuron and limbic system modulation are the mechanisms involved in visceral hypersensitivity. Enteric inflammatory cells may also play an important role in the pathophysiology of Irritable Bowel Syndrome. Clinicians have for many years recognized that the onset of IBS often follows an episode of acute gastroenteritis. Inflammation may alter intestinal cytokine milieu and motility, both of which can result in an increase in a patient’s pain sensation. The menstrual cycle may also affect gut sensation and motility. Other factors, such as malabsorption of sugars (lactose, fructose, and sorbitol), probably aggravate underlying IBS, rather than serving as root causes of the disorder. In patients with rapid transit times, short or medium chain fatty acids can reach the right colon and cause diarrhea.
Symptoms:
The hallmark of IBS is abdominal pain or discomfort associated with either a change in bowel habits or disordered defecation. The pain or discomfort associated with IBS is often poorly localized and may be migratory and variable. It may occur after a meal, during stress or at the time of menses. In addition to pain and discomfort, altered bowel habits are common, including diarrhea, constipation, and diarrhea alternating with constipation. Patients also complain of bloating or abdominal distension, mucous in the stool, urgency, and a feeling of incomplete evacuation. Some patients describe frequent episodes, whereas others describe long symptom-free periods. Patients with irritable bowel frequently report symptoms of other functional gastrointestinal disorders as well, including chest pain, heartburn, nausea or dyspepsia, difficulty swallowing, or a sensation of a lump in the throat or closing of the throat. Patients with IBS are generally classified according to the type of bowel habits that accompany pain. Some patients have diarrhea-predominant symptomatology, others constipation-predominant, and still others have a combination of the two. Some patients alternate between different subgroups. Symptoms may vary from barely noticeable to debilitating, at times within the same patient. In some patients, stress or life crises may be associated with the onset of symptoms, which may then disappear when the stress dissipates. Other patients seem to have random IBS episodes with spontaneous remissions. Still others describe long periods of symptoms and long symptom-free periods. In general, the symptoms of IBS wax and wane throughout life, but the majority of patients seen by physicians is 20–50 years old. In approximately 50% of patients, symptoms begin before age 35. The disorder is also recognized in children, generally appearing in early adolescence. Many patients can trace the onset of symptoms back to childhood. The prevalence of IBS is slightly lower in the elderly, and in this patient population organic disorders must be excluded. Extraintestinal symptoms are common in patients with IBS. These may include headache, sleep disturbances, post-traumatic stress disorder, temporomandibular joint disorder, sicca syndrome, back/pelvic pain, myalgias, back pain, and chronic pelvic pain. Fibromyalgia and interstitial cystitis are also frequently encountered in patients with IBS. In fact, Fibromyalgia occurs in up to 33% of patients with IBS and almost half of patients with fibromyalgia also have IBS.
The autonomic nervous systems and the bowel:
Sympathetic (red dashed) and parasympathetic (blue) nervous system innervate the gastrointestinal tract. Both carry sensory stimuli, though it appears that spinal afferent nerves in the dorsal horn of the spinal cord process pain. 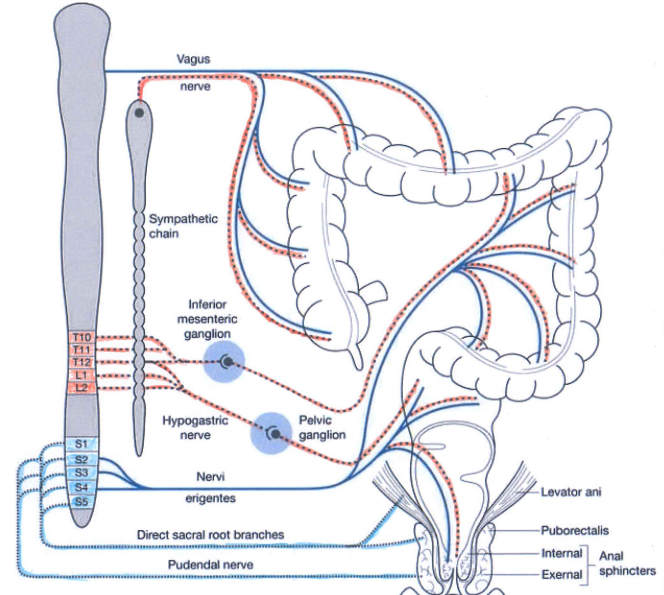
In normal conditions the sympathetic nervous system is active during the stress ( fight and flight and fright system) and the parasympathetic is more active during the rest ( rest and digest system).
Sympathetic activation produces:
1) Increased heart rate and cardiac muscle contractility and bronchodilation of the lungs.
2) Constriction of blood vessels in many parts of the body, especially in the bowels and vasodilation of the muscle vessels.
3) Inhibition of stomach and intestinal action to the point where digestion slows down or stops, the same is for defecation and urination.
4) General effect on the sphincters of the body.
5) Paling or flushing, or alternating between both.
6) Liberation of nutrients (particularly fat and glucose) for muscular action.
7) Inhibition of the lacrimal gland (responsible for tear production) and salivation.
8) Dilation of pupil (mydriasis).
9) Relaxation of bladder.
10) Inhibition of erection.
11) Auditory exclusion (loss of hearing).
12) Tunnel vision (loss of peripheral vision).
13) Disinhibition of spinal reflexes; and shaking
14) Increased glucose production and mobilization by the liver
15) Increased lipolysis within fat tissue.
Parasympathetic activation produces:
1) In the stomach and intestines, parasympathetic stimulation leads to increased motility and relaxation of sphincters and increased gastric secretions to aid in digestion.
2) Parasympathetic stimulation leads to vasodilation of internal blood vessels, especially intestinal vasculature.
3) In the gallbladder, parasympathetic stimulation induces contraction to release bile.
4) In the pancreas, parasympathetic stimulation leads to the release of digestive enzymes and insulin
5) In salivary glands, parasympathetic stimulation leads to high volume secretion of potassium ions, water, and amylase
6) In the heart, parasympathetic stimulation, causes decreased heart rate and velocity of conduction through the AV node.
7) In the eye, parasympathetic stimulation, causes contraction of the sphincter muscle of the iris, leading to constriction of the pupil (miosis). Additionally, it causes contraction of the ciliary muscle, improving near vision.
8) In the lungs, parasympathetic stimulation of M3 receptors leads to bronchoconstriction. It also increases bronchial secretions.
9) In the kidneys and bladder, parasympathetic stimulation, stimulates peristalsis of ureters, contraction of the detrusor muscle, and relaxation of the internal urethral sphincter aiding in the flow and excretion of urine.
10) Smooth muscle relaxation in the helicine arteries of the penis, allowing blood to fill the corpora cavernosa and corpus spongiosum, causing an erection. The PNS also gives excitatory signals to the vas deferens, seminal vesicles, and prostate.
Current research on the topic suggests a biopsychosocial model of the disorder, implicating physiological, emotional, behavioral and cognitive factors. Approximately 40–60% of patients with IBS who seek medical care also report psychiatric symptoms, such as depression, anxiety, or somatization. Interestingly, however, psychiatric symptoms in patients with IBS in the general population are not as prevalent. It is thought that these psychiatric disturbances influence coping skills and illness-associated behaviors. A history of abuse (physical, sexual, or emotional) has been correlated with symptom severity. More than half of patients who are seen by a physician for Irritable Bowel Disease report stressful life events coinciding with or preceding the onset of symptoms. Stress is known to alter gastrointestinal function. Patients who suffer from IBS have amplified colonic motility responses when compared to normal volunteers (those who do not have any symptoms of IBS).
We believe the limbic system (an area of the brain where stress is perceived and experienced and recorded) is critically involved. The majority of these recordings are not available in the conscious mind. In everyday life each event is processed between conscious mind and limbic system and the ultimate response is evaluated between past experiences and actual information received and then the final reaction is decided. If the limbic system is in stress mode or imbalanced mode all consecutive behaviour of autonomic nervous system will be abnormal.
Diagnosis :
In the absence of definitive diagnostic markers, the diagnosis of IBS rests on physician’s recognition of classic clinical symptoms and the exclusion of other diseases. To facilitate comparisons among different populations and assist in epidemiological studies of IBS, two sets of criteria for diagnosis have been developed—the Manning and Rome Criteria. A multinational working team subsequently developed the Rome Criteria. The original criteria, Rome 1, were recently revised and the new Rome 2 diagnostic criteria are included below.
Manning Criteria:
Abdominal pain that is relieved with a bowel movement.
Pain associated with more frequent stools.
Sensation of incomplete evacuation.
Passage of mucous.
Abdominal distension.
Rome Criteria
Continuous or recurrent symptoms
of:
Abdominal pain, relieved with defecation, or associated with change in frequency or consistency of stool
and/or
Disturbed defecation( two or more of):
Altered stool frequency
Altered stool form (hard or loose/watery)
Altered stool passage (straining or urgency, feeling of incomplete evacuation)
Passage of mucus
usually with bloating or feeling of abdominal distension
Revised Rome Criteria (65)
At least 12 weeks or more, which need not be consecutive, in the preceding 12 months of abdominal disconfort or pain that has two out of three features:
-Relieved with defecation
and/or
-Onset associated with a change in frequency of
and/or
-onset associated with a change in form(appearance) of stool
Symptoms that cumulatively support the diagnosis of irritable bowel syndrome
-Abnormal stool frequency(for reasurches puposes “abnormal” may be defined as greater than 3 bowel movements per day and less than three bowel movements per week
– Abnormal stool form
lumpy/hard or loose/waterystool)
-Abnormal stool passage( straining, urgency, or feeling of incomplete evacuation)
-Passage of mucus
-Bloating or feeling of abdominal distension
Diagnostic Approach
Effective diagnosis of IBS begins with a careful history and physical examination. The initial evaluation should also include: a complete blood count, chemistry panel, and erythrocyte sedimentation rate as well as a careful study of food allergies and a stool test for fecal occult blood . A colonoscopy should be performed in patients to exclude other types of bowel diseases. Once a diagnosis of IBS has been made, attention should be shifted to treatment. Continued investigations due to persistent symptoms are not warranted and may ultimately undermine a patient’s confidence in both the disorder diagnosis and the attending physician.
Therapy Overview
Management of patients with Irritable Bowel Syndrome is based on a positive diagnosis of the syndrome, exclusion of organic disorders, and specific therapies. Treatment for IBS should address the three main pathophysiologically important factors : psychosocial disturbances, visceral hypersensitivity, and dysmotility. Treatment should be patient oriented and geared towards symptom–specific relief. The majority of conventional IBS treatments currently used is empiric and has not been formally reviewed and scientifically approuved. Therapies may include fiber consumption for constipation, anti-diarrheals, smooth muscle relaxants for pain, and psychotropic agents for pain, diarrhea and depression. Patients with mild or infrequent symptoms may benefit from the establishment of a physician-patient relationship, patient education and reassurance, dietary modification, and simple measures such as fiber consumption. Patients with constipation-predominant IBS can generally be treated with osmotic mild laxatives. Stronger laxatives should be reserved for patients who do not respond to fiber consumption and gentle osmotic laxatives.
Physician-Patient Relationship :