What is a stem cell?
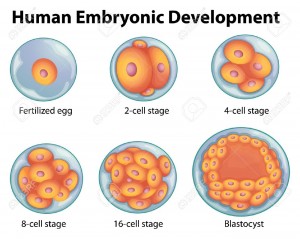
Ultimately, every cell in the human body can be traced back to a fertilized egg that came into existence from the union of egg and sperm. But the body is made up of over hundreds of different types of cells. All of these cell types come from a pool of stem cells in the early embryo. During early development, as well as later in life, various types of stem cells give rise to the specialized or differentiated cells that carry out the specific functions of the body, such as blood, muscle,bone and nerve cells.
Stem cells can regenerate themselves or produce specialized cell types. This property make stem cells appealing for scientists seeking to create medical treatments that replace lost or damaged cells.
TYPES OF STEM CELLS :
Stem cells are found in all of us, from the early stages of human development to the end of life. All stem cells may prove useful for medical research, but each of the different types has both promise and limitations. Embryonic stem cells, which can be derived from a very early stage in human development, have the potential to produce all of the body’s cell type. Adult stem cells, which are found in certain tissues in fully developed humans, from babies to adults, may be limited to producing only certain types of specialized cells. Recently, scientists have also identified stem cells in umbilical cord blood and the placenta that can give rise to the various types of blood cells.
Embryonic Stem Cells :
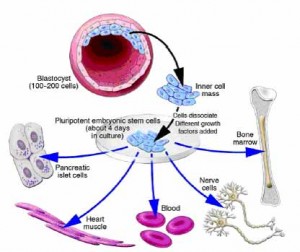
A blastocyst, is a pre-implantation embryo that develops 5 days after the fertilization of an egg by a sperm. It contains all the material necessary for the development of a complete human being. The blastocyst is a mostly hollow sphere. In its interior is the inner cell mass, which is composed of 30-34 cells that are referred to by scientists as pluripotent because they can differentiate into all of the cell types of the body.
In normal development, the blastocyst would implant in the wall of the uterus to become the embryo and continue developing into a mature organism. Its outer cells would begin to from the placenta and the inner cell mass would begin to differentiate into the progressively more specialized cell types of the body.
When the blastocyst is used for stem cell research, scientists remove the inner cell masse and place these cells in a culture dish with a nutrient-rich liquid where they give rise to embryonic stem cells. Embryonic stem cells seem to be more flexible than stem cells found in adults, because they have the potential to produce every cell type in the human body. They are also generally easier to collect, purify and maintain in the laboratory than adult stem cells. Scientists can induce embryonic stem cells to replicate themselves in an undifferentiated state for very long periods of time before stimulating them to create specialized cells. This means that just a few embryonic stem cells can build a large bank of stem cells to be used in experiments. However, such undifferentiated stem cells could not be used directly for tissue transplants because they can cause a type of tumor called a teratoma. To be used for therapies, embryonic stem cells would first need to be differentiated into specialized cell types.
Some find embryonic stem cell research to be morally objectionable, because when scientists remove the inner cell mass, the blastocyst no longer has the potential to become a fully developed human being.
Sources of Embryonic Stem Cells (In Vitro Fertilization):
The largest potential source of blastocysts for stem cell research is from in vitro fertilization (IVF) clinics. The process of IVF requires the retrieval of a woman’s eggs via a surgical procedure after undergoing an intensive regimen of “fertility drugs,” which stimulate her ovaries to produce multiple mature eggs. When IVF is used for reproductive purposes, doctors typically fertilize all of the donated eggs in order to maximize their chance of producing a viable blastocyst that can be implanted in the womb. Because not all the fertilized eggs are implanted, this has resulted in a large bank of “excess” blastocysts that are currently stored in freezers around the country. The blastocysts stored in IVF clinic could prove to be a major source of embryonic stem cells for use in medical research. However, because most of these blastocysts were created before the advent of stem cell research, most donors were not asked for their permission to use these left-over blastocysts for research.
The in vitro fertilization (IVF) technique could potentially also be used to produce blastocysts specifically for research purposes. This would facilitate the isolation of stem cells with specific genetic traits necessary for the study of particular diseases. For example, it may be possible to study the origins of an inherited disease like cystic fibrosis using stem cells made from egg and sperm donors who have this disease. The creation of stem cells specifically for research using IVF is, however, ethically problematic for some people because it involves intentionally creating a blastocyst that will never develop into a human being.
Nuclear Transfer:
The process called nuclear transfer offers another potential way to produce embryonic stem cells. In animals, nuclear transfer has been accomplished by inserting the nucleus of an already differentiated adult cell-for example, a skin cell-into a donated egg that has had its nucleus removed. This egg, which now contains the genetic material of the skin cell, is then stimulated to form a blastocyst from which embryonic stem cells can be derived. The stem cells that  are created in this way are therefore copies or “clones” of the original adult cell because their nuclear DNA matches that of the adult cell.
are created in this way are therefore copies or “clones” of the original adult cell because their nuclear DNA matches that of the adult cell.
As of the summer of 2006, nuclear transfer has not been successful in the production of human embryonic stem cells, but progress in research suggests that scientists may be able to use this technique to develop human stem cells in the future.
Producing Embryonic Stem Cells Using Nuclear Transfer Is Not the Same as Reproductive Cloning
The use of nuclear transfer to develop disease-specific stem cells can be called research cloning, and the use of this technique for personalized tissue transplants is sometimes called therapeutic cloning. These terms must be carefully distinguished from reproductive cloning, in which the intent is to implant a cloned embryo in a female’s womb and allow it to develop fully into an individual. This was the technique by which Dolly the sheep was made and is now widely used for reproductive cloning in animals. In humans, however, reproductive cloning has been actively discouraged by most in the scientific community.
Scientists believe that if they are able to use nuclear transfer to derive human stem cells, it could allow them to study the development and progression of specific diseases by creating stem cells containing the genes responsible for certain disorder. In the future, scientists may also be able to create “personalized” stem cells that contain only the DNA of a specific patient. The embryonic stem cells created by nuclear transfer would be genetically matched to a person needing a transplant, making it far less likely that the patient’s body would reject the new cells than it would be with traditional tissue transplant procedures.
Although using nuclear transfer to produce stem cells is not the same as reproductive cloning, some are concerned about the potential misapplication of the technique for reproductive cloning purposes. Other ethical considerations include egg donation, which requires informed consent, and possible destruction of blastocysts.
Adult Stem Cells :
Adult stem cells are hidden deep within organs, surrounded by millions of ordinary cells, and may help replenish some of the body’s cells when needed. In fact, some adult stem cells are currently being used in therapies. They have been found in several organs that need a constant supply of cells, such as the blood, skin and lining of the gut, and have also been found in surprising places like the brain, which is not known to readily replenish its cells. Unlike embryonic stem cells, adult stem cells are already somewhat specialized. For example, blood stem cells normally only give rise to the many types of blood cells, and nerve stem cells can only make the various types of brain cells. Recent research however, suggests that some adult stem cells might be more flexible than previously thought, and may be made to produce a wider variety of cells types. For example, some experiments have suggested that blood stem cells isolated from adult mice may also be able to produce liver, muscle and skin cells, but these results are not yet proven and have not been demonstrated with human cells. Nevertheless, scientists are working on finding a way to stimulate adult stem cells, or even other types of adult cells, to be more versatile. If they succeed, it could provide another source of unspecialized stem cells.
Identifying Stem Cells :
As early as 1961, scientists knew that adult bone marrow contained cells that could make all of the blood cell types. But it wasn’t until 1988 that those stem cells were isolated as pure populations. Why did it take so long? The techniques for identifying stem cells have only recently been developed. Partly, this is because adult stem cells are, by their very nature, inconspicuous in shape, size and function. They also tend to hide deep in tissues and are present only in very low numbers, making their identification and isolation like finding a needle in a haystack.
How do scientists know when they have found a stem cell? Every cell displays an array of proteins on its surface; different cell types have different proteins. Scientists can use these surface proteins as “markers” that characterize individual cell types – a type of molecular ID. For example, using molecules that recognize and attach to specific surface proteins and that can fluoresce under certain wavelengths of light, scientists can visually tell the difference between a blood cell. Unfortunately, not all stem cells can now be identified in this manner because scientists have not yet identified markers for all stem cell types. Scientists also identify stem cells by observing their behavior in the laboratory: stem cells must be able to remain unspecialized and self-renew for long periods of time.
Scientists believe that there might be more types of adult stem cells than the handful that have already been identified, but finding them is a difficult process.
Culturing Cell Lines and Stimulating Stem Cells to Differentiate
Cell culture is a term that refers to the growth and maintenance of cells in a controlled environment out-side of an organism. A successful stem cell culture is one that keeps the cells healthy, dividing and unspecialized. The culturing of stem cells in the first step in establishing a stem cell line – a propagating collection of genetically identical cells. Cell lines are important because they provide a long-term supply of multiplying cells that can be shared among scientists for research and therapy development. The National Academies report Stem Cells and the Future of Regenerative Medicine (2001) described some of the challenges of maintaining cell lines: “Over time, all cell lines…change, typically accumulating harmful genetic mutations. There is no reason to expect stem cell lines to behave differently. While there is much that can be learned using existing stem cell lines…such concerns necessitate continued monitoring of these cells as well as the development of new stem cell lines in the future.”
Once they have established a stable stem cell line, scientists start the process of causing the stem cells to differentiate into specialized cell types. The cellular environment in which stem cells naturally reside provides scientists with clues about how to make them differentiate in a culture dish. For example, in the bone marrow, where blood stem cells reside, bone cells send physical and chemicals signals that tell the blood stem cells when to differentiate. Scientists are just beginning to understand these signals and have developed ways to mimic the natural processes in cell cultures. Usually, the technology involves adding certain proteins to the cell culture and, in some cases, introducing specific genes into the stem cells.
It will be essential that scientists are sure that stem cells have fully differentiated before they can use them for medical applications. If completely undifferentiated stem cells (such as embryonic stem cells) are implanted directly into an organism, they can cause a type of tumor called a teratoma, which scientists have observed in experiments using mice. Semi-specialized adult stem cells and differentiated cells derived from embryonic stem cells are unlikely to cause teratomas.
Alternatives to Using Embryos in Stem Cell Research
To address ethical concerns about the destruction of blastocysts, scientists are trying to find new ways of obtaining stem cells that behave like embryonic stem cells but that don’t require harming a blastocyst. As the science progresses, ethical issues surrounding these alternatives may also arise. Some possible alternatives include:
1) Cells collected from the morul, the developmental stage prior to the blastocyst. The morula, a solid ball of about 16-30 cells, seems able to sustain the loss of a few cells without developmental damage so that the remaining cells can continue to develop. Cell extraction from the morula is already being used in some clinics to screen for genetic disorders in embryos produced by in vitro fertilization. Researchers have recently shown that cells isolated from a mouse morula can give rise to embryonic stem cells while the remaining morula cells develop into a healthy mouse. However, this process may still be morally objectionable to some because of the chance of harm to the morula, and because the long-term effects of removing cells from a morula are not yet known.
2) The creation of embryonic stem cells through a process called altered nuclear transfer (ANT). In this variation of the nuclear transfer technique, scientists create a blastocyst create whose genetic material has been changed so that further development and implantation into the uterus is not possible. It aims to create embryo-like entities that are not truly embryos but that can be a source of pluripotent stem cells. ANT, so far only tested with mouse blastocysts, could allow the creation of embryonic stem cells without destroying a viable human blastocyst. Some who object to embryonic stem cell research support ANT because the resulting blastocyst could never develop into a full human being and therefore would not have the moral status of a human embryo. However, this procedure is objectionable to some because they believe that it involves the creation of an imperfect blastocyst that is designed to be destroyed.
3) Causing an adult cell to act like an embryonic stem cell. During development, as cells become more and more specialized, they gradually lose the ability to turn on the genes that allow embryonic stem cells to be so versatile. The silencing if these genes seems to be responsible for keeping specialized cells specialized and limiting the differentiation capacities of adult stem cells. By “reprogramming” adult stem cells so that they can turn on the genes that allow versatility, scientists hope to cause them to revert to a more flexible state. It is even possible that scientists could one day “reprogram” any cell, not only stem cells. However, research in this area is in the early stages and scientists may be many years away from making an adult cell as versatile as an embryonic stem cell.